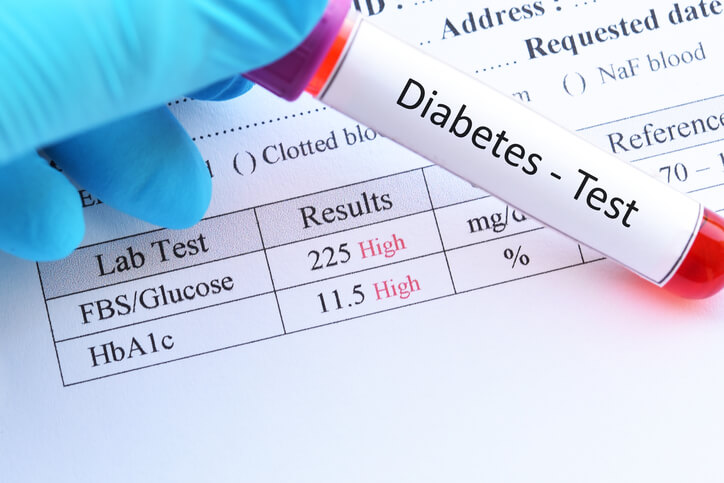
Daily blood sugar tests can help type 2 diabetics monitor their readings for unusual spikes and plateaus. However, these tests don’t provide long-term information about your overall health as a diabetic. For this reason, your doctor may conduct a blood test that measures your average blood sugar level every 2-3 months. It’s called the A1C test (or the hemoglobin A1C test, in some cases). It gives your physician an accurate view about how well your type 2 diabetes medication works to lower A1C levels.
In the past, doctors told patients to aim for an HbA1C (glycosylated hemoglobin) level between 6.5% and 7%. But the American College of Physicians (ACP) recently said doctors can aim to keep patients’ A1C levels somewhere between 7%-8%. These new goals affect type 2 diabetics using various medications to manage their disease. Especially since not all type 2 diabetes drugs are equally effective at achieving lower A1C readings recommended under previous guidelines.
What New ADA Guidelines to Lower A1C Mean for Type 2 Diabetics
The new guidelines published by the ACP gives four major recommendations for doctors treating type 2 diabetics:
- Personalize each type 2 diabetes patient’s goals for optimal blood sugar control. Goals should factor in medication’s benefits and harms, patient preferences, overall health and life expectancy, treatment burden, and out-of-pocket cost.
- Aim to lower A1C levels with medication until the patient achieves a number between 7%- 8%, in most cases.
- Consider reducing drug therapy in patients with much lower A1C levels than the recommended guidelines (i.e., less than 6.5%).
- Treat patients as needed to help minimize low blood sugar symptoms. Doctors should also avoid targeting a lower A1C level in patients whose current life expectancy is 10 years or less. This is because the risks outweigh the benefits for targeting a lower A1C in such patients. Patients should regularly check their blood sugar at home; we like the Care Touch glucose monitoring kit.
Why Are the New Guidelines To Lower A1C Levels So Controversial?
While the new guidelines come from a trusted source, the decision to set an easier-to-achieve blood sugar goal remains controversial. According to Reuters, multiple doctors stated that this new range is “inconsistent with guidelines from most national and international organizations.” Others feel relaxing the goal sends the wrong message to patients about health benefits that come with lower A1C levels. After all, there is no one-size-fits-all A1C reading, since patients and drug regimens vary.
Endocrinologist Dr. Rekha Kumar expressed concern about the way patients achieve this new goal — through drugs that help lower A1C. Dr. Kumar says, “I also don’t think pharmacotherapy should also be reduced in all patients who achieve a blood glucose average of 6.5% or under, especially because this A1C target may have been achieved on two new classes of medicines that treat type 2 diabetes — the GLP-1 receptor agonists and SGLT-2 inhibitors — which have shown a reduction in cardiovascular mortality.”
It’s true that various diabetes drugs lower A1C levels to a different degree in each patient. And while some do help regulate blood glucose levels, they also have other potentially damaging health effects, Dr. Kumar notes.
Below are the most commonly prescribed drugs to treat type 2 diabetes, and how much they help lower A1C levels.
Drug #1 to Lower A1C Levels: Empagliflozin (Jardiance)
Jardiance is an SGLT2-inhibitor, a popular drug class doctors prescribe to lower blood sugar. SGLT2 inhibitors cause your kidneys to remove extra sugar from your blood through urine.
Patients using Jardiance generally saw a reduction in A1C <1%. There is also a slight hypoglycemia risk with this medication and is the first drug shown to reduce cardiovascular event risks in patients. (This is one consideration Dr. Kumar expressed concerned about with the newest A1C guidelines.)
Drug #2 to Lower A1C Levels: Canagliflozin (Invokana)
Invokana is a common SGLT2-inhibitor doctors prescribe to help type 2 diabetics regulate blood sugar. Studies show Invokana can significantly reduce A1C levels. Nearly half the patients (45%) taking Invokana 100 mg. vs. a placebo achieved an A1C level <7% in 26 weeks. And 62% met the goal taking once-daily 300 mg. Invokana for 26 weeks.
However, Invokana also comes with some serious risks. The 2017 CANVAS-R study found Invokana more than doubled risks for lower-limb amputations among type 2 diabetics. The most common body parts lost to amputation are the patient’s toe and mid-foot. But some patients lost their entire leg to diabetic amputation. Others had multiple amputations, sometimes involving both feet. In May 2017, the FDA released an Invokana black box warning about its doubled risk for diabetic amputations, especially lost toes. A black box warning is the FDA’s most serious and highest warning level available for dangerous drugs and medical devices.
Drug #3 to Lower A1C Levels: Sitagliptin (Januvia)
Januvia is a DDP-IV inhibitor. This drug increases incretin levels, which in turn inhibits glucagon release. This increases insulin secretion, decreases gastric emptying, and decreases blood glucose levels.
Multiple clinical trials show Januvia effectively lowers A1C levels an average .8% within six months after starting treatment. (Researchers reported this average reduction in patients with a baseline 8.1% A1C reading.)
Drug #4 to Lower A1C Levels: Liraglutide (Victoza)
Victoza is a GLP-1 agonist. GLP-1 drugs work in a similar way to DDP-IV inhibitors, but much more potent. One 26-week study compared Victoza 1.2 mg against a drug containing 100 mg. sitagliptin combined with metformin. Researchers found this combo helped lower A1C levels better than its competitors, Januvia and Trulicity. This combination formula can also aid some type 2 diabetics with weight loss.
While these drugs may help you achieve your A1C goals, they can also come with some serious risks. Doctors should weigh the pros and cons before prescribing drugs solely for lowering A1C levels. Invokana can cause ketoacidosis, stroke, kidney damage, and significantly increased risk for lost toes, feet and legs in diabetic patients.
How to Get Justice and Compensation for Lost Toes, Feet or Legs
If you or someone you love took Invokana or Invokamet and lost a toe, foot or leg, you may qualify for a cash settlement. To check your eligibility for compensation, take two minutes to fill out your free Invokana claim review form today. Once you’ve submitted your information, an experienced lawyer will call you to discuss how to get the compensation and justice you deserve.
Related: Off Label Invokana Use: Is It Really Worth Risking Your Life?
Mandy Voisin
Mandy Voisin is a freelance writer, blogger, and author of Girls of the Ocean and Star of Deliverance. As an accomplished content marketing consultant, mom of four and doctor's wife, Mandy has written hundreds of articles about dangerous drugs and medical devices, medical issues that impact disabled Americans, veterans' healthcare and workers' compensation issues since 2016.